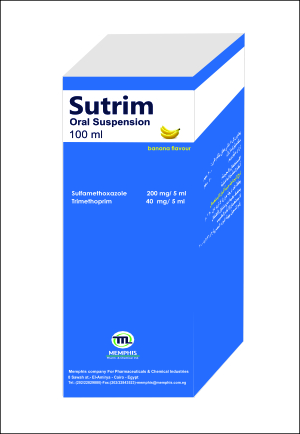
Sulfamethoxazole 200 mg/Trimethoprim 40 mg oral SUSPENSION 1-NAME OF THE MEDICINAL PRODUCT SUTRIM 2- QUALITATIVE AND QUANTITATIVE COMPOSITION: Each 5 ml of suspension contains: Active ingredient: Sulfamethoxazole Micronized (D90 < 30 pm) 200 mg Trimethoprim Micronized (D90 < 30 pm) 40 mg Excipients: Carboxy methyl cellulose (CMC sodium), Avicel RC 591, Polyvinyl Pyrolidine (PVP k17), Colloidal silicone dioxide, Methyl paraben, Sodium benzoate, Glycerin, Propylene glycol, Sorbitol 70% solution, Tween 80, Banana BC 401, Sucralose, Citric acid, Purified water. 3-PHARMACEUTICAL FORM: Oral suspension Creamy white homogenous suspension after shaking,with banana odour. 4-CLINICAL PARTICULARS 4.1 INDICATIONS: Sutrim Suspension is indicated in children aged 12 years and under (infants (>3 months to <2 years old) children (>2 to <12 years old) for the treatment of the following infections when owing to sensitive organisms: Treatment and prevention of Pneumocystis jirovecii pneumonitis (PJP). Treatment and prophylaxis of toxoplasmosis. Treatment of nocardiosis. The following infections may be treated with Sutrim where there is bacterial evidence of sensitivity to (Sulfamethoxazole /Trimethoprim) and good reason to prefer the combination of antibiotics in Sutrim to a single antibiotic: Acute uncomplicated urinary tract infection. Acute otitis media. Acute exacerbation of chronic bronchitis. Consideration should be given to official guidance on the appropriate use of antibacterial agents. 4.2- POSOLOGY AND METHOD OF ADMINISTRATION: Posology: Standard dosage recommendations for acute infections Children aged 12 years and under (infants (>3 months to < 2 years old) and children (>2 to <12 years old) The standard dosage for children is equivalent to approximately 6 mg trimethoprim and 30 mg sulfamethoxazole per kg body weight per day, given in two equally divided doses. The schedules for children are according to the child’s age and provided in the table below: STANDARD DOSAGE Age Paediatric Suspension 6 to 12 years 10 ml every 12 hours. 6 months to 5 years 5 ml every 12 hours. 3 months to 5 months 2.5 ml every 12 hours. Treatment should be continued until the patient has been symptom free for two days; the majority will require treatment for at least 5 days. If clinical improvement is not evident after 7 days therapy, the patient should be reassessed. As an alternative to Standard Dosage for acute uncomplicated lower urinary tract infections, short-term therapy of 1 to 3 days duration has been shown to be effective. Impaired hepatic function: No data are available relating to dosage in patients with impaired hepatic function. Impaired renal function: Dosage recommendation: Adults (>18 years old) and children over 12 years old (>12 to <18 years old): Creatinine Clearance (ml/min) Recommended Dosage >30 10 ml every 12 hours 15 to 30 5 ml every 12 hours <15 Not recommended No information is available for children aged 12 years and under with renal failure. See PHARMACOKINETICS section for the pharmacokinetics in the paediatric population with normal renal function of both components of Sutrim TMP and SMZ. Measurements of plasma concentration of sulfamethoxazole at intervals of 2 to 3 days are recommended in samples obtained 12 hours after administration of Sutrim. If the concentration of total sulfamethoxazole exceeds 150 microgram/ml then treatment should be interrupted until the value falls below 120 microgram/ml. Pneumocystis jirovecii pneumonitis: Treatment - Children aged 12 years and under (infants (>3 months to < 2 years old) and children (>2 to <12 years old): A higher dosage is recommended, using 20 mg trimethoprim and 100 mg sulfamethoxazole per kg of body weight per day (see table below) in two or more divided doses for two weeks. The aim is to obtain peak plasma or serum levels of trimethoprim of greater than or equal to 5 microgram/ml (verified in patients receiving 1-hour infusions of intravenous TMP and SMZ). Prevention - Children aged 12 years and under (infants (>3 months to < 2 years old) and children (>2 to <12 years old): The standard dosage for children is equivalent to approximately 6 mg trimethoprim and 30 mg sulfamethoxazole per kg body weight per day, given in two equally divided doses. The schedules according to the child’s age that may be used for the duration of the period at risk are provided in the table below: Age Paediatric Suspension 6 to 12 years 10 ml every 12 hours, seven days per week 6 to 12 years 10 ml every 12 hours, three times per week on alternative days 6 to 12 years 10 ml every 12 hours, three times per week on consecutive days 6 to 12 years 20 ml once a day, three times per week on consecutive days 6 months to 5 years 5 ml every 12 hours, seven days per week 6 months to 5 years 5 ml every 12 hours, three times per week on alternative days 6 months to 5 years 5 ml every 12 hours, three times per week on consecutive days 6 months to 5 years 10 ml once a day, three times per week on consecutive days 3 months to 5 months 2.5 ml every 12 hours, seven days per week 3 months to 5 months 2.5 ml every 12 hours, three times per week on alternative days 3 months to 5 months 2.5 ml every 12 hours, three times per week on consecutive days 3 months to 5 months 5 ml once a day, three times per week on consecutive days The daily dose given on a treatment day approximates to 150 mg trimethoprim/m2/day and 750 mg sulfamethoxazole/m2/day. The total daily dose should not exceed 320 mg trimethoprim and 1600 mg sulfamethoxazole. Nocardiosis: There is no consensus on the most appropriate dosage. Adult doses of 6 to 8 tablets daily for up to 3 months have been used (one tablet contains 400 mg sulfamethoxazole and 80 mg trimethoprim). For doses cannot be achieved by Sutrim oral SUSPENSION use other suitable pharmaceutical formulations for (Sulfamethoxazole /Trimethoprim ) Toxoplasmosis: There is no consensus on the most appropriate dosage for the treatment or prophylaxis of this condition. The decision should be based on clinical experience. For prophylaxis, however, the dosages suggested for prevention of Pneumocystis jirovecii pneumonitis may be appropriate. Method of administration: Oral. It may be preferable to take Sutrim with some food or drink to minimise the possibility of gastrointestinal disturbances. 4.3-CONTRAINDICATIONS: Hypersensitivity to the active substance(s) sulphonamides, trimethoprim, Sutrim or to any of the listed excipients. Severe impairment of liver. Patients with severe renal insufficiency where repeated measurements of the plasma concentration cannot be performed. Sutrim should not be given to patients with a history of drug-induced immune thrombocytopenia with use of trimethoprim and/or sulphonamides. Sutrim should not be given to patients with acute porphyria. Sutrim should not be given to infants during the first 3 months of life. 4.4-WARNINGS AND PRECAUTIONS FOR USE: Life-threatening adverse reactions FATALITIES ASSOCIATED WITH THE ADMINISTRATION OF SULFONAMIDES, ALTHOUGH RARE, HAVE OCCURRED DUE TO SEVERE REACTIONS INCLUDING STEVENS-JOHNSON SYNDROME, TOXIC EPIDERMAL NECROLYSIS, FULMINANT HEPATIC NECROSIS, AGRANULOCYTOSIS, APLASTIC ANAEMIA, OTHER BLOOD DYSCRASIAS, ACUTE AND DELAYED LUNG INJURY, HYPERSENSITIVITY OF THE RESPIRATORY TRACT, AND CIRCULATORY SHOCK. Life-threatening cutaneous reactions Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN) and drug reaction with eosinophilia and systemic symptoms (DRESS) have been reported with the use of trimethoprim/sulfamethoxazole. Patients should be advised of the signs and symptoms and monitored closely for skin reactions. The highest risk for occurrence of SJS or TEN is within the first weeks of treatment. If symptoms or signs of SJS, TEN (e.g. progressive skin rash often with blisters or mucosal lesions) or DRESS (e.g. fever, eosinophilia) are present, Sutrim treatment should be discontinued. The best results in managing SJS, TEN and DRESS come from early diagnosis and immediate discontinuation of any suspect drug. Early withdrawal is associated with a better prognosis. If the patient has developed SJS, TEN and DRESS with the use of Sutrim, Sutrim must not be re-started in this patient at any time. At the start of treatment, the occurrence of a generalised febrile erythema associated with pustules, should raise the suspicion of acute generalised exanthematous pustulosis (AGEP); it requires cessation of treatment and contraindicates any new administration of Sutrim alone or in combination with other drugs. Haemophagocytic lymphohistiocytosis (HLH ) Cases of HLH have been reported very rarely in patients treated with trimethoprim/sulfamethoxazole. HLH is a life-threatening syndrome of pathologic immune activation characterised by clinical signs and symptoms of an excessive systemic inflammation (e.g. fever, hepatosplenomegaly, hypertriglyceridaemia, hypofibrinogenaemia, high serum ferritin, cytopenias and haemophagocytosis). Patients who develop early manifestations of pathologic immune activation should be evaluated immediately. If diagnosis of HLH is established, Sutrim treatment should be discontinued. Respiratory toxicity Very rare, severe cases of respiratory toxicity, sometimes progressing to Acute Respiratory Distress Syndrome (ARDS), have been reported during co-trimoxazole treatment. The onset of pulmonary signs such as cough, fever, and dyspnoea in association with radiological signs of pulmonary infiltrates, and deterioration in pulmonary function may be preliminary signs of ARDS. In such circumstances, co-trimoxazole should be discontinued and appropriate treatment given. Other severe pulmonary adverse reactions occurring within days to week of trimethoprim-sulfamethoxazole initiation and resulting in prolonged respiratory failure requiring mechanical ventilation or extracorporeal membrane oxygenation (ECMO), lung transplantation or death have also been reported in patients and otherwise healthy individuals treated with trimethoprim-sulfamethoxazole products. Circulatory shock Circulatory shock with fever, severe hypotension, and confusion requiring intravenous fluid resuscitation and vasopressors has occurred within minutes to hours of re-challenge with trimethoprim-sulfamethoxazole in patients with history of recent (days to weeks) exposure to sulfamethoxazole-trimethoprim. Acute respiratory failure including acute eosinophilic pneumonia has been reported in healthy adolescents with sulfamethoxazole/trimethoprim treatment. Elderly patients Particular care is always advisable when treating older patients because, as a group, they are more susceptible to adverse reactions and more likely to suffer serious effects as a result particularly when complicating conditions exist, e.g. impaired kidney and/or liver function and/or concomitant use of other drugs. Patients with renal impairment For patients with known renal impairment special measures should be adopted. Urinary output An adequate urinary output should be maintained at all times. Evidence of crystalluria in vivo is rare, although sulphonamide crystals have been noted in cooled urine from treated patients. In patients suffering from malnutrition the risk may be increased. Folate Regular monthly blood counts are advisable when Sutrim is given for long periods, or to folate deficient patients or to older patients; since there exists a possibility of asymptomatic changes in haematological laboratory indices due to lack of available folate. Supplementation with folinic acid may be considered during treatment but this should be initiated with caution due to possible interference with antimicrobial efficacy. Patients with glucose-6-phosphate dehydrogenase deficiency In glucose-6-phosphate dehydrogenase (G-6-PD) deficient patients, haemolysis may occur. Patients with severe atopy or bronchial asthma Sutrim should be given with caution to patients with severe atopy or bronchial asthma. Treatment of streptococcal pharyngitis due to Group A beta-haemolytic streptococci Sutrim should not be used in the treatment of streptococcal pharyngitis due to Group A beta-haemolytic streptococci; eradication of these organisms from the oropharynx is less effective than with penicillin. Phenylalanine metabolism Trimethoprim has been noted to impair phenylalanine metabolism but this is of no significance in phenylketonuric patients on appropriate dietary restriction